Preventing Rectal Prolapse: A Surgeon’s Advice
Do you often feel an uncomfortable bulge in your rectum? For many individuals, this is not a passing worry. Rather, a troublesome symptom caused by a condition called rectal prolapse.
It occurs when the rectum (the last section of the large intestine) loses its normal attachments, causing it to slide out through the anal orifice and turn inside out. Rectal prolapse is an extremely uncomfortable, distressing and progressive situation.
The condition primarily affects the older population who are above 50 years of age, especially women, who are six times more likely to get it than men.
Rectal prolapse surgery is an effective solution providing lasting relief from the symptoms and discomfort. However, there are countless patients who ask, “Could I have something to prevent the worsening of the condition in the first place?”
Let’s know below.
Rectal Prolapse: An Overview
As stated, rectal prolapse is a medical condition where the rectum, the final segment of the large intestine, loses its normal support structure and begins to slip or protrude through the anus. While it may start mildly, rectal prolapse is typically progressive, meaning it tends to worsen over time if not properly managed.
There are 3 types of rectal prolapse, which are as follows:
- The whole rectum protrudes out of the anus.
- The rectal lining is only partially pushed into the anus.
- The rectum begins to descend, but it does not stretch beyond the anus.
Rectal prolapse is often misdiagnosed as haemorrhoids, particularly in its early stages. While both conditions affect the rectal area and may share some similar symptoms, such as a bulge, bleeding, or discomfort, they are different and require different treatment approaches.
Rectal prolapse is caused by the slipping of the attachments of the final section of the large intestine. On the other hand, haemorrhoids are enlarged blood vessels that form in the lower rectum and anus.
As a result, some patients mistake the condition and continue to apply haemorrhoid creams with little or no improvement. Hence, always make sure to consult a skilled surgeon like Dr. Purnendu Bhowmik for proper evaluation and, if required, undergo rectal prolapse surgery without delay.
What Are The Symptoms?
The warning signs usually vary depending on the severity of the condition. Some of the common symptoms:
- A feeling of pressure, bulge or protrusion in your anus.
- A feeling like there’s something left inside your anus after you poop.
- A red, fleshy mass hanging out of your anus.
- Leakage of mucus, poop or blood from your anus.
- Anal pain or itching.
- Pain and discomfort when sitting
Although rectal prolapse surgery is a reliable option, there are ways in which you can prevent the progression of the disease. But first, we will delve into the risk factors that make a patient prone to developing the disease.
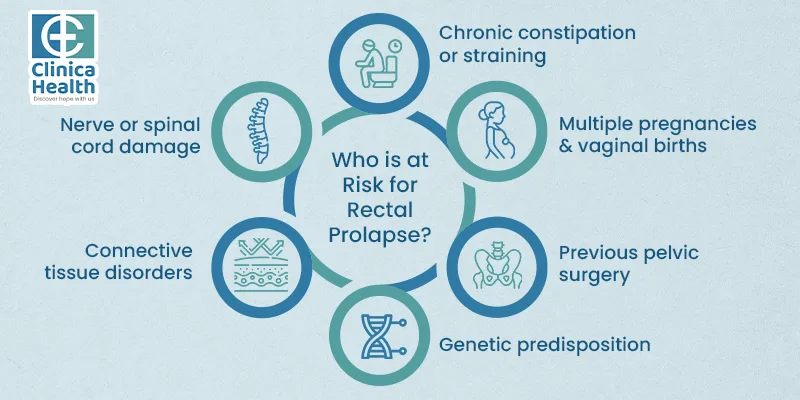
Who Is At Risk?
According to Dr. Purnendu Bhowmik, the best surgeon for rectal prolapse, several factors increase the chance of the condition.
- Chronic constipation or straining during bowel movements is a major risk
- Age, especially women who are above the age of 50 years.
- Multiple pregnancies and vaginal births weaken the pelvic floor muscles.
- Previous pelvic surgery
- Genetic predisposition
- Connective tissue disorders
- Frequent coughing or diarrhoea
- Nerve or spinal cord damage
- Cystic fibrosis
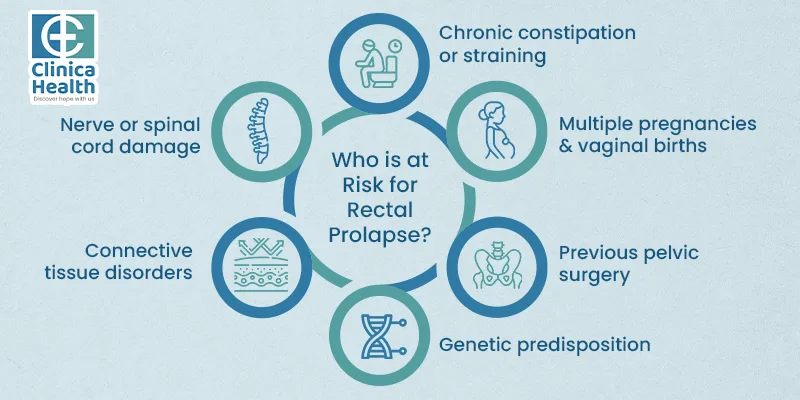
The earlier the risks are identified and addressed, the better the chance of progression.
Rectal Prolapse Prevention Tips
Here are the following measures you can follow to delay the need for rectal prolapse surgery.
- Maintain healthy bowel habits.
Constant straining during bowel movements is one of the reasons for rectal prolapse. Whether it is due to constipation or poor bowel habits, the repeated pressure weakens the pelvic muscles over time. Hence, Dr. Purnendu Bhowmik urges patients to adopt natural bowel movements to prevent constipation. For instance,
- Don't delay the urge to go.
- Avoid prolonged sitting on the toilet
- Eat foods that are rich in fibre, such as fruits, vegetables, legumes and whole grains.
- Drink plenty of water and fluids
- Use stool softeners if required.
- Engage in regular exercise.
Aim for at least 30 minutes of exercise every day to strengthen the pelvic floor muscles. Regular constriction and relaxation support the rectum and other pelvic organs. For example, you can practice 3 sets of Kegels every day; however, avoid them during urination. Consulting a trained specialist or surgeon proves to be beneficial, as they can help you with the right technique.
Obesity, particularly abdominal obesity, is a major factor that increases intra-abdominal pressure and weakens the pelvic floor. Dr. Purnendu Bhowmik advises patients to maintain a normal BMI. If you are overweight, aim to lose body weight by adopting a balanced diet and regular physical activity. Weight loss is quite important in managing constipation and bowel function.
- Avoid strenuous activities
Excessive heavy lifting or intense abdominal workouts can worsen the pelvic muscles and increase the risk of their onset. Instead, follow proper lifting techniques or wear supportive garments when engaging in labour-intensive activities. This will help to minimise strain on the pelvic and rectal structures.
Women who have had multiple vaginal pregnancies are more likely to develop rectal prolapse later in life. This is primarily due to the stretching or injury to the pelvic floor muscles and connective tissues. Hence, take proper postpartum care by incorporating pelvic floor exercises, avoiding heavy lifting and managing constipation.
When Does Surgery Become Necessary?
Despite the best efforts, some patients still develop rectal prolapse. In such situations, rectal prolapse surgery becomes a part of the treatment plan. Here are the signs to watch for.
- Persistent or worsening prolapse despite conservative care
- Fecal incontinence
- Rectal bleeding or ulceration
- Incomplete bowel movements or obstruction
Modern minimally invasive surgical techniques are completely safe with improved outcomes, no complications and reduced recurrence.
Conclusion
Rectal prolapse is a serious condition, but it is treatable with rectal prolapse surgery. If you suspect the disease or are suffering from persistent rectal discomfort, don’t wait. Get in touch with an experienced surgeon like Dr. Purnendu Bhowmik for both preventive measures and timely intervention.
 Call Now:
8010 552 552
7595 838 844
Call Now:
8010 552 552
7595 838 844
 Whatsapp Now:
8010 552 552
Whatsapp Now:
8010 552 552
 Email Me:
[email protected]
Email Me:
[email protected]