-
 Call Now:
8010 552 552
7595 838 844
Call Now:
8010 552 552
7595 838 844
-
 Email Me:
clinicahealthkolkata@gmail.com
Email Me:
clinicahealthkolkata@gmail.com
An anal fistula is a tunnel connecting an infected cyst in the anus to an opening on the skin surrounding the anus. When small glands that produce mucous inside the anus get clogged and infected, it forms abscess or cyst, explains Dr. Purnendu Bhowmik, the best fistula doctor in Kolkata. Half of these abscesses have a chance of developing into a fistula.
The leading cause of an anal fistula is clogged anal glands that produce mucous and anal abscesses. Other rare conditions that can lead to the development of anal fistula are:
Symptoms that indicate Anal Fistula are:
If you experience the above symptoms, visit Clinica Health for the best fistula treatment in Kolkata
Yes. It must be treated because it doesn’t heal on its own. There is also a risk of developing cancer in the fistula tract if left untreated for a long period of time.
Yes. A well planned and well executed fistula surgery by the best proctologist in Kolkata can offer complete cure. Most fistulas are simple to treat. But few may pose difficulty when they are complex in nature.
Surgery is the only effective treatment for an anal fistula.
The laser surgery for fistula or FiLaC is a minimally invasive surgery in the treatment of anal fistulas. As per the Fistula Surgeon, Fistula Laser Closure (FiLaC) is comparatively new surgical technique in which the fistulous tract is ablated using a ‘radial laser fibre’ resulting in destruction of the fistula walls and granulation tissue followed by shrinkage and subsequent closure of the tract.
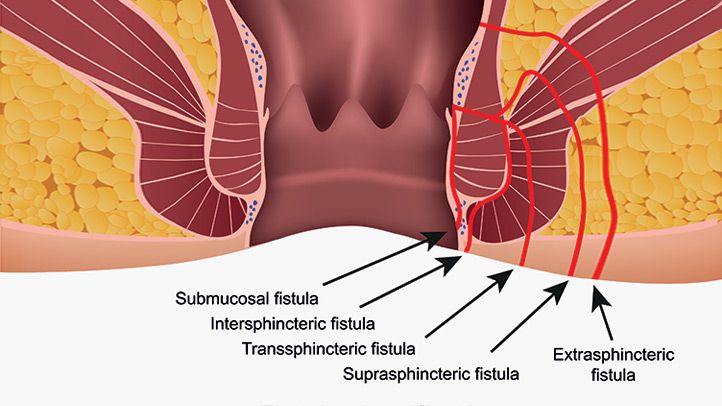
Clinica Health provides effective and safe fistula laser treatment in Kolkata. Laser closure of the fistula is a painless treatment and is effective in the case of transsphinteric anal fistula. A conventional surgical procedure, in this case, carries the risk of injury to the anal sphincter (circular muscle), resulting in post-surgery faecal incontinence.
Conventional fistula surgery usually takes about 6 – 8 weeks to recover. However, laser fistula treatment only takes a few days to recover and patients can get back to their regular activities.
| Sl No. | Factors | Conventional Surgery | Laser Surgery |
|---|---|---|---|
| 1 | Hospital Stay | 3-5 days | Daycare, no stay |
| 2 | Pain | Intense (3-4 wks) | Painless |
| 3 | Bleeding During Surgery | Moderate | Bloodless |
| 4 | Ability to SIt after Operation | No/Difficult Sitting for 4wks | Can Sit from 2nd Day |
| 5 | Wound | Moderate to Large | No Obvious Wound |
| 6 | Healing | 2 months approx | Few Days |
| 7 | Medication | Long Course | 5-7 Days |
| 8 | Anal Stenosis | Yes | No |
| 9 | Relief of Constipation after Surgery | No | Yes |

My fistula problem was giving me a lot of trouble for long. Finally found Dr. Bhowmik through one of my friend. Found him as good as I heard about him. And at last, a laser procedure cured me of my long standing problem. He is the best laser surgeon in Kolkata…

My fistula was making my life a hell for so many years. Operated twice earlier in other centres and it recurred within 2-3 months everytime. This time I found Dr. Bhowmik from one of my close contact. I was suffering so badly that I just requested him to get myself out of it. He did laser fistula surgery…

Underwent laser fistula surgery by Dr.Purnendu. It was a satisfying experience even in this covid time. Now I am free from a disease I was suffering for so long. Thank you doctor.
Anal fistula is a an abnormal communication between the anorectal canal and the perianal skin that is lined with granulation tissue. It occurs as a result of an anorectal abscess, which was previously drained. While the abscess is the acute phase of the disease, fistula represents the chronic phase.
Infection of the glands in the intersphincteric space between the EAS and IAS is thought to be the primary cause of both acute anorectal abscesses and anal fistulas —the ‘cryptoglandular hypothesis’, described by the best fistula doctor in Kolkata.
When it comes to diagnosing fistula anatomy, MRI is considered the “gold standard”.
The cumulative incidence of anal fistula in patients with Crohn’s disease is 20-25%. Fistulas are often complex and multiple; this makes the treatment difficult. In this case, anti-tumor necrosis factor-α therapy is considered the first-line treatment. Surgical options are considered if medical treatment fails, but because of the poor rate of wound healing in active Crohn’s disease, a defunctioning colostomy is a more common strategy.
Tuberculosis may be the cause of anal fistula in some cases, says the fistula doctor. Tuberculosis should be suspected in patients who fail to respond to standard treatment or who develop recurrent fistulas. Diagnosis is made through the histological finding of granulomatous disease and the positive identification of acid fast bacilli. Antituberculous drugs are the first line treatment.
Mon to Sat: 8 am – 5 pm, Sunday: CLOSED